The following is an original article published by the Frontiers in Public Health last November 19, 2020. It was written by Quentin De Larochelambert, Andy Marc, Juliana Antero, Eric Le Bourg, and Jean-François Toussaint.
The researchers performed statistical analysis to determine the potential associations between COVID-19 mortality in the first 8 months of 2020 and major indices such as demography, public health, economy, politics, and environment. The study included 160 countries, as well as several individuals states in the US and China, which accounted for a total of 846,395 deaths due to COVID up to the study end point (August 31, 2020).
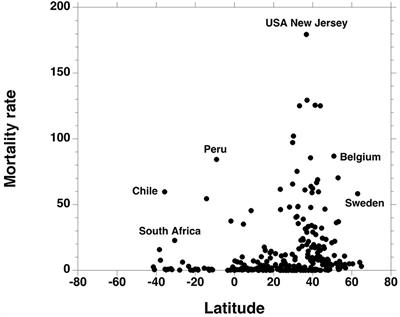
The authors offered the following conclusion for their study: “higher Covid-19 mortality rates are mostly found in countries experiencing higher life expectancies and showing a recent slowdown of this progression. Most of these developed and aging societies are latitudinally located over the 25° parallel. They also have higher GDP and chronic diseases levels (e.g., CVD and cancer) associated with major metabolic risk factors (e.g., inactive lifestyle, sedentarity, and obesity). High temperature and UV levels are associated with low death rates such that northern and western countries pay the most severe toll to Covid-19.”
Through the Principal Component Analysis, the researchers also found a strong correlation between COVID-19 death rate obesity which may mean that inactive lifestyles can lead to higher death toll. Lockdowns and the stringency of government measure for pandemic control were not associated with the death rate of COVID-19.
Editor’s Note: Several studies have shown previously that lockdowns have no meaningful effect on controlling COVID-19 death rates [we have an entire category dedicated to this topic, see Is a lockdown necessary?].
What makes the study different from others we have seen before is that it has started the conversation about the factors that affect COVID-19 mortality. And the research has showed us exactly what we have been expecting all along: over all health plays a major role. Continued focus on health can help prevent deaths, which is only logical, especially since COVID-19 is a health issue and must be given evidence-based health-focused solutions.
Since the beginning of the pandemic, experts have been saying that poor countries are most vulnerable from the virus, but the results of this study shows otherwise. The discovery that deaths are much larger in countries with high-GDP and high incidence of chronic diseases is a bit surprising. While this is a welcome development, it leads us to ask an important question: what is the difference in terms of health systems of rich and poor countries?
Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation
Context: The human development territories have been severely constrained under the Covid-19 pandemic. A common dynamics has been observed, but its propagation has not been homogeneous over each continent. We aimed at characterizing the non-viral parameters that were most associated with death rate.Methods: We tested major indices from five domains (demography, public health, economy, politics, environment) and their potential associations with Covid-19 mortality during the first 8 months of 2020, through a Principal Component Analysis and a correlation matrix with a Pearson correlation test. Data of all countries, or states in federal countries, showing at least 10 fatality cases, were retrieved from official public sites. For countries that have not yet finished the first epidemic phase, a prospective model has been computed to provide options of death rates evolution.Results: Higher Covid death rates are observed in the [25/65°] latitude and in the [−35/−125°] longitude ranges. The national criteria most associated with death rate are life expectancy and its slowdown, public health context (metabolic and non-communicable diseases (NCD) burden vs. infectious diseases prevalence), economy (growth national product, financial support), and environment (temperature, ultra-violet index). Stringency of the measures settled to fight pandemia, including lockdown, did not appear to be linked with death rate.Conclusion: Countries that already experienced a stagnation or regression…
https://www.frontiersin.org/article/10.3389/fpubh.2020.604339/full
Read Offline
Click the button below if you wish to read the article offline.
